Know Your Brain: Phantom Limb
Background
In the 16th century, an eminent French barber surgeon named Ambroise Pare noted—with amazement—that some of his patients who had undergone limb amputation complained months later that they still felt sensations (including pain) coming from their missing limb. Pare’s observation is thought to be the first recorded description of phantom limb, a condition in which sensations continue to occur in a part of the body that has been lost (due to accident or injury) or surgically removed. Despite the name, phantom limb doesn’t only occur in limbs, and has also been recorded after the loss or removal of other parts of the body—like breasts, genitals, and even teeth.
Although Pare wrote about phantom limb in the 1500s, the term phantom limb wouldn’t first be used until the Civil War—more than three centuries later. At that time, the renowned physician Silas Weir Mitchell was an army surgeon stationed at the South Street Hospital in Philadelphia. So many amputees were treated at South Street Hospital (especially after the Battle of Gettysburg) that soldiers called it “Stump Hospital.” Mitchell noted that most of the amputees he treated there continued to experience sensations from their missing limbs. He described these lingering sensations as “sensory ghosts” or “phantoms,” which led to the use of the term phantom limb to describe the condition.
Today, phantom sensations are recognized as a common experience in those who have lost a limb. It’s thought that almost all amputees have phantom sensations, and the majority of them also suffer from some degree of phantom pain. In one study of 5000 American veterans, for example, 78% of them reported experiencing phantom pain in their amputated limbs.
The presentation of phantom sensations can vary from patient to patient. In most cases, the sensations begin almost immediately after the surgery or injury that led to the loss of the limb (after consciousness has returned and any anesthetic has worn off). But in about a quarter of patients, the sensations may not appear for several days or weeks. Sometimes the phantom sensations fade away after a few days or weeks, but in other cases they persist for years—or even decades.
In many patients, the phantom limb takes on a habitual posture (e.g., arm slightly bent). But that posture may change spontaneously, and some patients complain that their phantom limb ends up in awkward positions that generate discomfort and pain. One anecdotal report describes a patient who lost a limb after a grenade exploded in it. He complained that his phantom hand was perpetually held in a painful, tightly-clenched fist.
What causes phantom limb?
Phantom limb is still not very well understood. A number of hypotheses have been proposed to explain it, but it’s likely that the underlying mechanism differs slightly from case to case. In this article, I’ll discuss a few of the most common explanations for phantom limb. In an individual patient, it’s very possible more than one of the following mechanisms is at play—or that other explanations altogether are involved.
Changes to the central nervous system
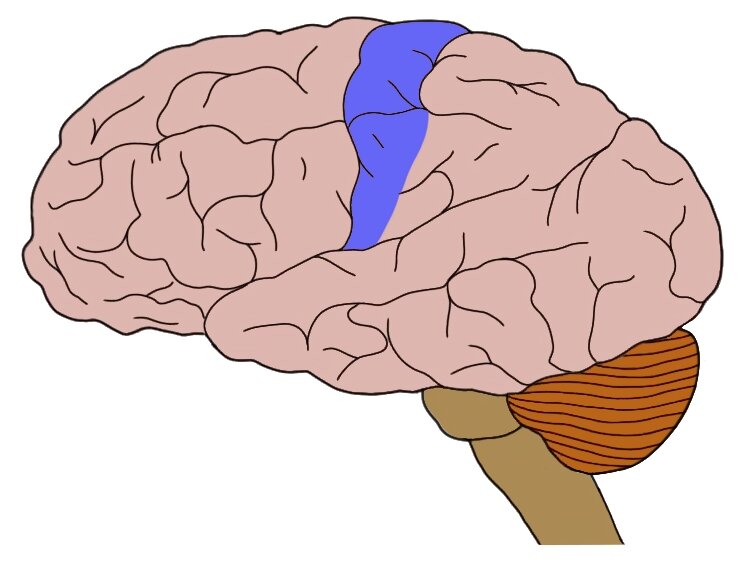
The prevailing explanation for phantom limb sensations is an idea known as cortical reorganization or cortical remapping. To explain this hypothesis, let’s consider the case of an individual who loses their arm in an accident. Before the accident, neurons that carried sensations from the arm communicated with neurons in a region known as the somatosensory cortex, which receives information about touch, pain, temperature, and proprioception (i.e., the position of the body in space) from all over the body. Specifically, neurons carrying information from the arm interact with neurons in a part of the somatosensory cortex devoted to processing information about arm sensations.
After the accident, however, those somatosensory neurons are deprived of their normal source of neuronal input. Consequently, they begin to respond to signaling from other nearby neurons. This can cause sensations felt in other parts of the body (e.g., the face) to lead to the stimulation of neurons in the somatosensory cortex that are devoted to the (now missing) arm. The activation of these “arm” somatosensory neurons causes the brain to perceive sensations in the arm, even though it is no longer there. The extent to which this type of maladaptive cortical reorganization occurs is correlated with the severity of phantom limb pain.
It should be noted that reorganization in non-cortical areas, like the thalamus (a subcortical structure involved in processing nearly all incoming sensory information) also seems to play a role in some phantom sensations.
Body representation
Another popular explanation for phantom limb centers around the idea that the brain typically relies on an internal representation of the body for generating an awareness of where our body is in space—and thus for maintaining posture, making movements, etc. This internal representation of the body is likely created by networks of neurons that integrate information of various types in the brain (e.g., tactile, visual—even emotional).
According to some researchers, the internal representation of the body can be the root of phantom limb sensations and pain. This might occur when, after a limb is lost, the body representation remains intact. In other words, the representation of the body generated in the patient’s brain still includes the intact limb, creating an expectation or sense that the limb is still present. This might lead to abnormal sensations, discomfort, or pain when incoming sensory information conflicts with the neural body representation (e.g., the eyes see that no leg is present, but the brain still expects a leg to be there).
Peripheral nervous system
In the early days of phantom limb research, the peripheral nervous system was thought to be the sole cause of phantom limb pain. Today, explanations typically involve the central nervous system as well, but the peripheral nervous system is still believed to be an important factor.
After the loss of a limb, the damaged axons that once supplied the limb don’t simply stay idle. Instead, they often attempt to repair themselves by growing new extensions (a process called sprouting). After loss of a limb, however, these new extensions essentially have nowhere to go. They form a mass of neural tissue at the site of amputation called a neuroma.
The axons that make up the neuroma do not remain dormant. Instead, they can generate action potentials in an erratic manner. This aberrant signaling is thought to be a potential mechanism underlying some of the spontaneous pain phantom limb patients can experience. The abnormal neural activity might be exacerbated by pathological signaling coming from the area where the axons from the missing limb enter the spinal cord.
Treatments for phantom limb pain
There are a number of pharmacological treatments for phantom limb pain. They include many of the same pain-relieving drugs used to treat other types of neuropathic pain, such as anticonvulsant and opioid drugs. The effectiveness of pharmacological treatment, however, tends to be variable—which likely reflects the numerous causes underlying phantom limb pain.
A patient holding a mirror to reflect his intact limb as part of mirror therapy.
One unique approach to treating phantom limb pain is called mirror therapy. In this technique, a mirror is situated between the missing and intact limb so it reflects the patient’s intact limb. This creates the illusion (from the patient’s perspective) that they have two intact limbs. They can move their intact limb and observe the illusory limb moving in the same manner. It is thought that this imagery may help to reduce some of the discomfort caused by the lack of visual feedback from a missing limb that the brain has maintained an internal representation of.
Although studies support the effectiveness of mirror therapy, the mechanisms underlying why the approach works are not fully understood. Some research, however, suggests mirror therapy may help to reverse the post-amputation cortical reorganization mentioned above. The effectiveness of mirror therapy has increased interest in similar approaches, like using virtual reality to create a representation of a limb.
References (in addition to linked text above):
Collins KL, Russell HG, Schumacher PJ, Robinson-Freeman KE, O'Conor EC, Gibney KD, Yambem O, Dykes RW, Waters RS, Tsao JW. A review of current theories and treatments for phantom limb pain. J Clin Invest. 2018 Jun 1;128(6):2168-2176. doi: 10.1172/JCI94003. Epub 2018 Jun 1. PMID: 29856366; PMCID: PMC5983333.
Flor H, Nikolajsen L, Staehelin Jensen T. Phantom limb pain: a case of maladaptive CNS plasticity? Nat Rev Neurosci. 2006 Nov;7(11):873-81. doi: 10.1038/nrn1991. PMID: 17053811.
Ramachandran VS, Hirstein W. The perception of phantom limbs. The D. O. Hebb lecture. Brain. 1998 Sep;121 ( Pt 9):1603-30. doi: 10.1093/brain/121.9.1603. PMID: 9762952.


