Know Your Brain: Aphasia
Background
In April of 1861, a 51-year old patient at the Bicetre Hospital in France was put under the care of a young surgeon named Paul Pierre Broca. The patient, Louis Victor Leborgne, was suffering from a gangrenous leg infection and near death. Broca had treated cases of gangrene like Leborgne’s before, but he became particularly interested in this case for another, unrelated aspect of Leborgne’s condition: Leborgne had a severe language deficit that made him unable to speak fluently—or indeed, much at all.
Leborgne had lived a difficult life, suffering from epilepsy from a young age and becoming hemiplegic (paralyzed on one half of the body) and bedridden in his 40s. He had begun to experience some cognitive impairment later in life, but when Broca met him Leborgne was still aware of what was going on around him and appeared to have thoughts that he wanted to communicate. Whenever he tried to do so, however, he was unable to get the words out. In fact, pretty much the only word he was able to articulate was “tan,” typically uttered in a repetitive chorus of “tan, tan.” Because of this he earned the nickname Tan in the hospital (and is still often referred to as Tan in many re-tellings of this story).
Leborgne died less than a week after he was put under Broca’s care, and Broca, intensely curious about what type of brain damage might produce this strange speech deficit, promptly conducted an autopsy. Broca noted damage to several areas of Leborgne’s brain—possibly the consequences of many years of seizures—but he found that the most substantial damage was to the left frontal lobe. Broca observed a pit in the left frontal lobe that he described as being about the size of a chicken’s egg.
After Leborgne, Broca identified a number of other cases with comparable speech abnormalities, and they all had damage to a similar area in the left frontal lobe—a region that would eventually come to be known as Broca’s area. Broca coined the term aphemia, which literally means “absence of speech,” to refer to the language deficit he studied. Soon after, however, another physician (Armand Trousseau) suggested the use of the term aphasia. For reasons that are unclear, aphasia is the name that stuck, and the disorder Broca observed in Leborgne came to be known as Broca’s aphasia (more on this below).
The diversity of symptoms associated with aphasia was expanded a little over a decade later, when a young German physician named Carl Wernicke described patients who had experienced damage to an area nearer to the back of the brain than Broca’s area—a region that would come to be known as Wernicke’s area. These patients displayed a qualitatively different language impairment than Broca’s patients. They had no trouble producing speech, but when they did, it didn’t make sense—they spoke mostly gibberish. And they suffered from impairments in understanding language as well. This disorder became known as Wernicke’s aphasia.
Since Broca and Wernicke’s discoveries in the 19th century, other cases have further broadened our definition of aphasia. Today, aphasia is an umbrella term that is associated with a variety of impairments in the expression, understanding, and/or communication of language (written, spoken, or other) that are acquired as a result of brain damage. The most common cause of aphasia is stroke, although there can be a number of other causes as well, ranging from head trauma to dementia.
Types of aphasia
There are a number of traditionally recognized types of aphasia, but it’s important to note that many aphasic patients have a collection of symptoms that don’t fit neatly into one of these categories. Additionally, the symptoms of aphasia are dynamic, and may change over time in an individual patient. Thus, the aphasic syndromes described below are useful as typical examples, but a particular case of aphasia may not always fit well within one of these categories. While these are some of the “classic” aphasic syndromes, there are a number of other recognized types of aphasia as well.
Patients with Broca’s aphasia have trouble producing fluent speech. Their symptoms might resemble those of Broca’s patient (Leborgne), and they may be restricted to a vocabulary of only one or two words. Or they might struggle with other aspects of fluent speech, like producing complete grammatical sentences or adding intonation to their words. Basic comprehension typically remains intact, although patients might have trouble when it comes to understanding more complex language structures, like sentences that use passive voice.
As mentioned above, patients with Wernicke’s aphasia tend to have no trouble producing fluent speech, but their speech often has little meaning. They might substitute one word for another, mix up the sounds within words, or even create new words altogether—in both spoken and written language. Some patients seem to speak with such ease that it appears they are competently speaking another language. Their ability to comprehend language is also impaired. Wernicke’s patients tend to be unaware of their language deficits, and can often be engaged in a conversation where they will offer meaningless responses and feign understanding for the duration of the discussion.
Global aphasia is a severe form of aphasia that involves a combination of the symptoms from Broca’s and Wernicke’s aphasia. Patients with global aphasia experience deficits in both the production and comprehension of speech. In some cases, they may be mute, and they typically retain little ability to understand both spoken and written language.
Patients with conduction aphasia are capable of producing fluent speech, but they often experience what are known as phonemic paraphasias. Phonemic paraphasias involve unintentionally replacing a word with a non-word that has some phonetic similarities to the intended word. For example, a patient trying to say “car” might say “dar.” Patients sometimes will go through a series of utterances that closely resemble what they’re trying to say before finally landing on the right word (e.g. “dar, far, tar, bar—car”). Language comprehension is typically intact.
In the transcortical aphasias, patients have deficits similar to what would be seen in other types of aphasia (e.g. they might have all of the symptoms of Broca’s aphasia), but they don’t exhibit the deficit when asked to repeat something. For example, a patient might have symptoms of Broca’s aphasia and be unable to produce a sentence—or even a few words—on his own. But if you asked him to repeat the sentence, “Cindy went to the store," he would be able to.
Finally, anomic aphasia primarily involves deficits in word retrieval—especially of nouns. Comprehension is good and patients have little trouble speaking fluently, but they struggle to remember certain words, like the names of objects. Many cases of aphasia have elements of anomic aphasia, but anomic aphasia occurs when word retrieval is the paramount problem. This tends to create a relatively mild disorder, as patients can generally still hold a conversation by describing objects instead of naming them. For example, when referring to a fork, a patient with anomic aphasia could say, “Hand me the pointy thing I can use to pick up my food.”
The aphasias are sometimes categorized by whether or not the patient is still able to speak fluently (regardless of how meaningful the speech is). Using this categorization, for example, Broca’s aphasia and global aphasia would be considered nonfluent aphasias, while Wernicke’s aphasia and conduction aphasia would be considered fluent aphasias.
Neuroscience of aphasia
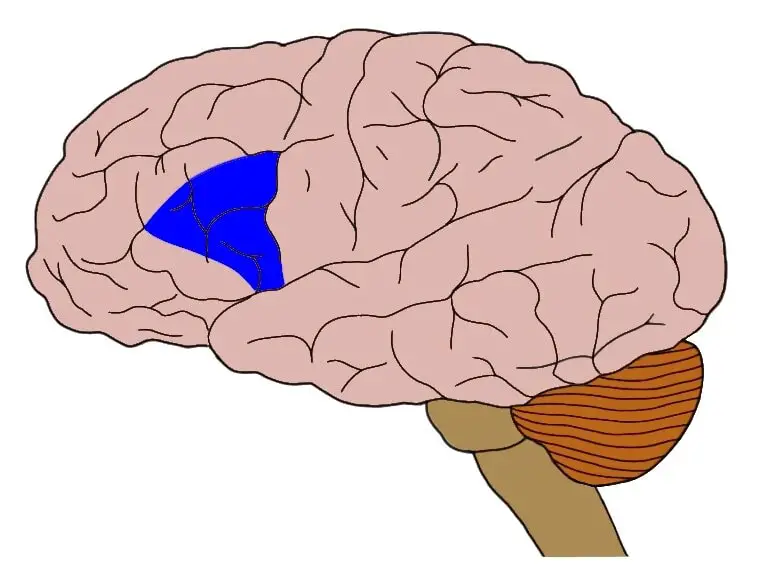
Prompted by the identification of presumed centers for language in the brain (e.g. Broca’s and Wernicke’s areas), Carl Wernicke devised a simple model of language function in the 1870s. Wernicke’s theory was modified several times over the years, but in some form it remained one of the predominant explanations for how language works in the brain for over a century. It suggests that Wernicke’s area is involved with language comprehension and providing meaning to language, while Broca’s area is involved with language production. According to this perspective, normal language function requires an interaction between these two regions. A popular adaption of Wernicke’s model (developed in the 1960s by neurologist Norman Geschwind) suggests the communication between Broca’s and Wernicke’s is primarily accomplished by one large bundle of neurons called the arcuate fasciculus, which stretches between the two regions.
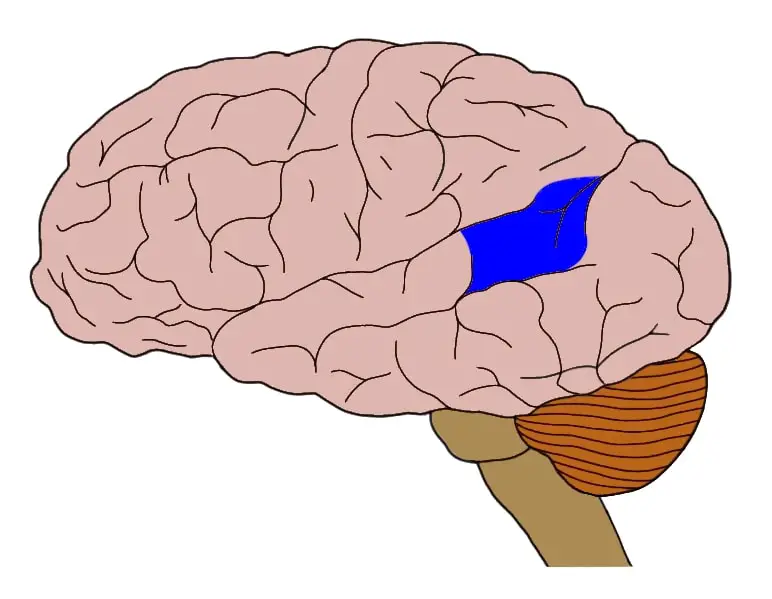
In this image, Broca’s area is represented by the blue region closer to the front of the brain (on the left), while Wernicke’s area is represented by the blue region closer to the back of the brain (on the right). The red lines represent the arcuate fasciculus, connecting the two regions.
Using this simple model, which I’ll hereafter refer to as the classic model of language, language deficits in the aphasias were attributed to straightforward neural counterparts. If someone was displaying symptoms of Broca’s aphasia, it was safe to assume she had damage to Broca’s area, and if she was displaying symptoms of Wernicke’s aphasia, she likely had suffered damage to Wernicke’s area. Other types of aphasia were attributed to damage to related structures (e.g. conduction aphasia was linked to damage to the arcuate fasciculus), or to the combined effects of damage to Broca’s and Wernicke’s areas (this was the widely-accepted explanation for global aphasia).
These simple designations, however, were never universally accepted, and after neuroimaging techniques like functional MRI (fMRI) were developed in the 1980s, criticisms of the classic model of language became difficult to ignore. Modern neuroimaging showed us that that neural structures underlying language are much more complex than just Broca’s and Wernicke’s area, just as language is much more complicated than just production and comprehension (there is a long list of other tasks involved in even the simplest language—ranging from word selection to the incorporation of syntax). Additionally, modern studies suggested that deficits in speech production or comprehension can be caused by damage to a number of different areas of the brain (not just Broca’s, Wernicke’s, and their connecting fibers). Similarly, healthy speech production and comprehension recruits many areas beyond those that Broca and Wernicke identified.
Thus, today it is recognized that the classic model of language is far too simple. And while, damage to language “centers” like Broca’s area and Wernicke’s area is common in the aphasias (with the location of the damage depending, to some degree, on the symptoms of aphasia seen), that damage is rarely localized to only these regions. For example, aphasia might also involve damage to various other parts of the brain like the insula, basal ganglia, thalamus, and so on. Each individual case of aphasia is different, and even very similar clinical symptoms might be linked to divergent types of brain damage.
So, although there are some common themes in the neuroanatomy of aphasias (like a tendency for damage to be associated with the left cerebral hemisphere), there is also a great deal of variation from case to case. Just as the symptoms of real aphasic disorders often do not neatly fit the clinical picture of aphasia we have created over the years, the neurological damage associated with aphasia cases does not often line up with the expectations created for us by Broca and Wernicke.
Clearly, our understanding of aphasia is still evolving. Fortunately, the majority of patients with most types of aphasia do recover substantially or completely. And, although our treatment options are limited, language therapy can significantly facilitate recovery. Still, researchers continue to explore this group of disorders not only to improve treatment of aphasic patients but also to develop a better understanding of how the brain creates and understands language.
References (in addition to linked text above):
Hillis AE. Aphasia: progress in the last quarter of a century. Neurology. 2007 Jul 10;69(2):200-13.
Willmes K, Poeck K. To what extent can aphasic syndromes be localized? Brain. 1993 Dec;116 ( Pt 6):1527-40.
Learn more: